Diet, Nutrition, and Lifestyle Interventions for Migraine Relief
Article from University of California, Irvine. Author: Dr Lilian Au, ND, MPH, SSIHI Naturopathic Doctor
Migraines are a common headache disorder but not all headaches are migraines. It is unlike any typical headache as it is a neurological condition that involves the release of pain and inflammatory substances from the blood vessels and nerves around the head, which can be triggered by diet, lifestyle, stress and environmental factors. Some of the common characteristics of migraines can be recognized as unilateral or bilateral pulsating head pain with attacks that can last hours to days and can be preceded by warning symptoms such as an aura, sensory disturbances that present as flashing lights, blind spots, or visual disturbances. They are also often associated with one or more of the following symptoms: dizziness, nausea, vomiting, numbness or tingling in the face or extremities, vision changes, sensitivity to light, smell, sound, and touch. Migraines can be extremely debilitating and have negative physical, social, mental, and financial impacts on quality of life and those affected are at higher risk for developing anxiety, depression, and/or co-morbid conditions such as obesity, irritable bowel syndrome, and celiac disease. The cause of migraines still remains poorly understood and there are various factors that may play a role in migraine pathology from diet and nutritional deficiencies, genetics, hormones, stress and environmental exposures.[1]
There are emerging integrative health approaches in migraine therapy that may help manage symptoms, reduce triggers, and alleviate pain. The current treatment of migraines often involves medication therapy, diet, and/or lifestyle modifications. There is growing evidence that dietary modifications, reducing environmental exposures, managing stress, and supplementation to correct nutrient deficiencies have prophylactic and therapeutic benefits on migraine prevention and treatment. [2]
The following interventions emphasize diet and lifestyle approaches to migraine headache management and prevention:
Maintain healthy eating patterns
Eating regularly at meal times or having small frequent meals throughout the day are associated with less frequent migraine headaches. Have a balanced meal with protein, carbohydrates, good fats, fruits, vegetables, and maintain adequate hydration. [3,4] Skipping meals or prolonged periods of time between meals may trigger or cause more severe migraine attacks due to hunger and low blood sugar levels.
Avoid specific food triggers
Although it may not affect everyone, dietary factors are commonly reported as triggers for migraine headaches. The International Classification of Headache Disorders III states that the ingestion of different substances can cause headaches immediately or within 12 hours of ingestion and resolve after 72 hours after ingestion. [5] Commonly reported triggers are caffeine, alcohol, aged cheeses, chocolate, and food preservatives with nitrites, nitrates, monosodium glutamate, tyramine, or artificial sweeteners such as aspartame and gluten. Recognizing and eliminating food or additives that provoke headaches may be beneficial for patients with migraines through food diary observation, elimination diets, or IgG food sensitivity testing, which may provide additional support in determining specific dietary triggers.[6] These types of diets can be considered under supervision of a medical provider and/or dietitian support as a comprehensive approach to identify and reduce migraine triggers, which are important for patient motivation, compliance, and success of therapy.
Support nutrient deficiencies through diet and supplementation
Nutrient deficiencies (vitamin B2, B6, B12, D, folate, magnesium, CoQ10, and polyunsaturated fatty acids) have been associated with perpetuating or exacerbating migraine headaches. The role of diet and nutrition in causing as well as treating migraine headache disorders have been widely studied around the mechanisms of action in brain energy metabolism associated with migraine pathophysiology, which focus on essential cofactor pathways, mitochondrial function and stabilization, anti- inflammatory response in the pain pathway, and antioxidant status. Diets rich in fresh fruits and vegetables, high in omega 3 fatty acids (fish, nuts, seeds), low fat, and plant-based with minimal intake of animal products have benefits in preventing and restoring nutrient deficiencies [7, 8]. Certain use of nutraceuticals such as vitamins (B2, B6, B12, D, folate), minerals (magnesium), antioxidants (CoQ10) and omega -3 fatty acids are essential nutrient cofactors that play a role in the prophylaxis of migraines and have been shown in studies to reduce the frequency and severity of episodes, minimize attacks, and have minimal adverse effects. [9, 10]
Minimize environmental exposures: weather changes, bright or flashing lights, odors, noise and air pollution (chemicals, perfumes, smog)
Migraine sufferers may have decreased thresholds and sensitivity to light, noise, olfactory and visual stimuli. Although few studies confirm environmental influences, given the impact of migraine disability on healthcare costs and productivity losses, preventive measures can be implemented within the home, work, or school environment to reduce potential exposures. [11]
Engage in healthy lifestyle behaviors
Get regular exercise at least 30 to 60 minutes daily, reduce alcohol consumption, avoid smoking, reduce stress through mindfulness practice, and maintain optimal sleep habits are moderating factors in migraine management. Establishing daily routines and self-regulated behaviors optimize physical, mental, and emotional health and have protective benefits in migraine prevention and treatment. [12,13]
Support nutrient deficiencies through diet and supplementation
Nutrient deficiencies (vitamin B2, B6, B12, D, folate, magnesium, CoQ10, and polyunsaturated fatty acids) have been associated with perpetuating or exacerbating migraine headaches. The role of diet and nutrition in causing as well as treating migraine headache disorders have been widely studied around the mechanisms of action in brain energy metabolism associated with migraine pathophysiology, which focus on essential cofactor pathways, mitochondrial function and stabilization, anti- inflammatory response in the pain pathway, and antioxidant status. Diets rich in fresh fruits and vegetables, high in omega 3 fatty acids (fish, nuts, seeds), low fat, and plant-based with minimal intake of animal products have benefits in preventing and restoring nutrient deficiencies [7, 8]. Certain use of nutraceuticals such as vitamins (B2, B6, B12, D, folate), minerals (magnesium), antioxidants (CoQ10) and omega -3 fatty acids are essential nutrient cofactors that play a role in the prophylaxis of migraines and have been shown in studies to reduce the frequency and severity of episodes, minimize attacks, and have minimal adverse effects. [9, 10]
Minimize environmental exposures: weather changes, bright or flashing lights, odors, noise and air pollution (chemicals, perfumes, smog)
Migraine sufferers may have decreased thresholds and sensitivity to light, noise, olfactory and visual stimuli. Although few studies confirm environmental influences, given the impact of migraine disability on healthcare costs and productivity losses, preventive measures can be implemented within the home, work, or school environment to reduce potential exposures. [11]
Engage in healthy lifestyle behaviors
Get regular exercise at least 30 to 60 minutes daily, reduce alcohol consumption, avoid smoking, reduce stress through mindfulness practice, and maintain optimal sleep habits are moderating factors in migraine management. Establishing daily routines and self-regulated behaviors optimize physical, mental, and emotional health and have protective benefits in migraine prevention and treatment. [12,13]
Our Holistic approach
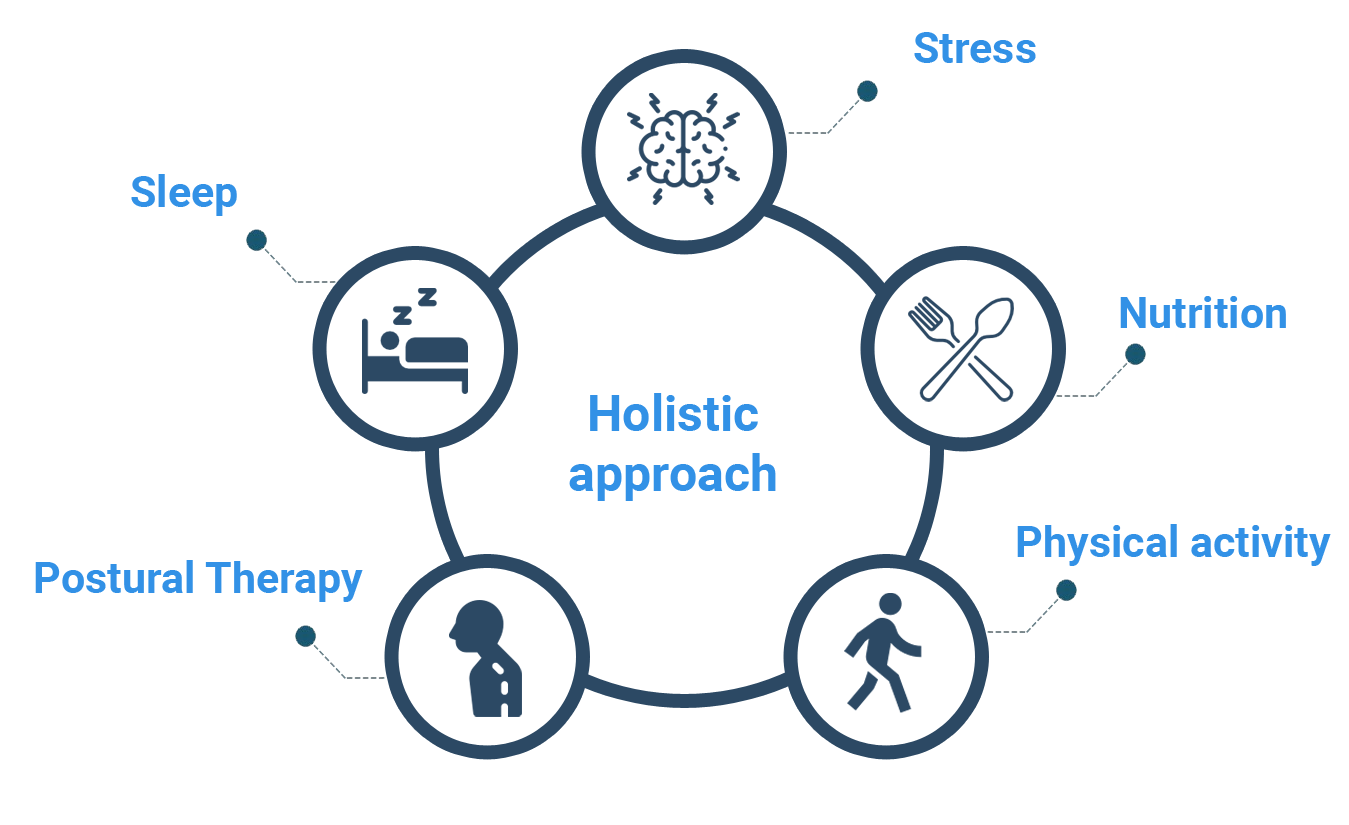
The Scandinavian Method uses a holistic approach. Through a thorough assessment we look for factors that is proven to cause migraine and tension-type headache. Here you can upload pictures of yourself and get help from our AI to analyze your posture.
After the assessment our system will create a personalized 90-days program. The program is science based and uses techniques that have been scientifically proven to reduce the intensity and frequency of migraine and headaches.
A holistic approach like this has also proven to help those who already are under medical treatments.
The program has been created by authorized health personell by the Norwegian government with over 15 years experience treating migraine and tension-type headache.
The Scandinavian Method is partly funded by the Norwegian government through Innovation Norway.
References
- F Gasparini, C., G Sutherland, H., & R Griffiths, L. (2013). Studies on the pathophysiology and genetic basis of migraine. Current genomics, 14(5), 300-315.
- Mollaoğlu, M. (2013). Trigger factors in migraine patients. Journal of health psychology, 18(7), 984-994.
- Jahromi, S. R., Ghorbani, Z., Martelletti, P., Lampl, C., & Togha, M. (2019). Association of diet and headache. The journal of headache and pain, 20(1), 1-11.
- Spigt, M. G., Kuijper, E. C., Van Schayck, C. P., Troost, J., Knipschild, P. G., Linssen, V. M., & Knottnerus, J. A. (2005). Increasing the daily water intake for the prophylactic treatment of headache: a pilot trial. European journal of neurology, 12(9), 715-718.
- Arnold, M. (2018). Headache classification committee of the international headache society (ihs) the international classification of headache disorders. Cephalalgia, 38(1), 1-211.
- Alpay, K., Ertaş, M., Orhan, E. K., Üstay, D. K., Lieners, C., & Baykan, B. (2010). Diet restriction in migraine, based on IgG against foods: a clinical double-blind, randomised, cross-over trial. Cephalalgia, 30(7), 829-837.
- Slavin, M., & Ailani, J. (2017). A Clinical Approach to Addressing Diet with Migraine Patients. Current neurology and neuroscience reports, 17(2), 17. https://doi.org/10.1007/s11910-017-0721-6
- Migraine. (2018). In Barnard, N. D. (Ed.), Nutrition Guide for Clinicians (3rd edition). Physicians Committee for Responsible Medicine. Retrieved November 09, 2020, from https://nutritionguide.pcrm.org/nutritionguide/view/Nutrition_Guide_for_Clinicians/1342056/all/Migraine
- Nattagh-Eshtivani, E., Sani, M. A., Dahri, M., Ghalichi, F., Ghavami, A., Arjang, P., & Tarighat-Esfanjani, A. (2018). The role of nutrients in the pathogenesis and treatment of migraine headaches. Biomedicine & Pharmacotherapy, 102, 317-325.
- Taylor, F. R. (2011). Nutraceuticals and headache: the biological basis. Headache: the journal of head and face pain, 51(3), 484-501.
- Friedman, D. I., & De Ver Dye, T. (2009). Migraine and the environment. Headache: The Journal of Head and Face Pain, 49(6), 941-952.
- Woldeamanuel, Y. W., & Cowan, R. P. (2016). The impact of regular lifestyle behavior in migraine: a prevalence case–referent study. Journal of neurology, 263(4), 669-676.
- Simshäuser, K., Lüking, M., Kaube, H., Schultz, C., & Schmidt, S. (2020). Is Mindfulness-Based Stress Reduction a Promising and Feasible Intervention for Patients Suffering from Migraine? A Randomized Controlled Pilot Trial. Complementary medicine research, 27(1), 19-30.