Understanding CGRP and Migraine
What is CGRP?
CGRP stands for Calcitonin Gene-Related Peptide. It’s a small protein in your body that acts as a neurotransmitter – essentially a chemical messenger that helps nerve cells communicate with each other. CGRP is found throughout your body, but it’s particularly important in the brain and the trigeminal nerve system, which is responsible for sensation in your face and head.
CGRP’s Role in Migraine
During a migraine attack, several things happen:
- CGRP Release: When a migraine begins, neurons in your brain release excessive amounts of CGRP.
- Blood Vessel Effects: CGRP causes blood vessels in the brain to dilate (widen), which contributes to the throbbing pain you feel during a migraine.
- Inflammation: CGRP triggers inflammation in the tissues surrounding nerves and blood vessels, making pain receptors more sensitive.
- Pain Signaling: CGRP enhances pain signals being sent to the brain, amplifying the migraine pain.
An interesting discovery was that people with migraine have higher levels of CGRP in their blood during an attack compared to when they’re headache-free. Even between attacks, migraine sufferers tend to have higher baseline CGRP levels than people who don’t get migraines.
CGRP Inhibitors: A Breakthrough in Migraine Treatment
Understanding the crucial role of CGRP in migraine led to the development of CGRP inhibitors. These are medications designed to either:
- Block CGRP Receptors: Some medications act like a key that doesn’t fit properly in a lock. They attach to the CGRP receptor but don’t activate it, preventing the real CGRP from binding.
- Bind to CGRP Itself: Other medications act like sponges that soak up excess CGRP, preventing it from reaching its receptors.
By interfering with CGRP’s actions, these medications can:
- Prevent migraines from occurring
- Reduce the severity and duration of migraines that do occur
- Decrease sensitivity to migraine triggers
CGRP inhibitors represent one of the most significant advances in migraine treatment in decades because they were specifically designed to target the underlying mechanism of migraine rather than just treating symptoms.
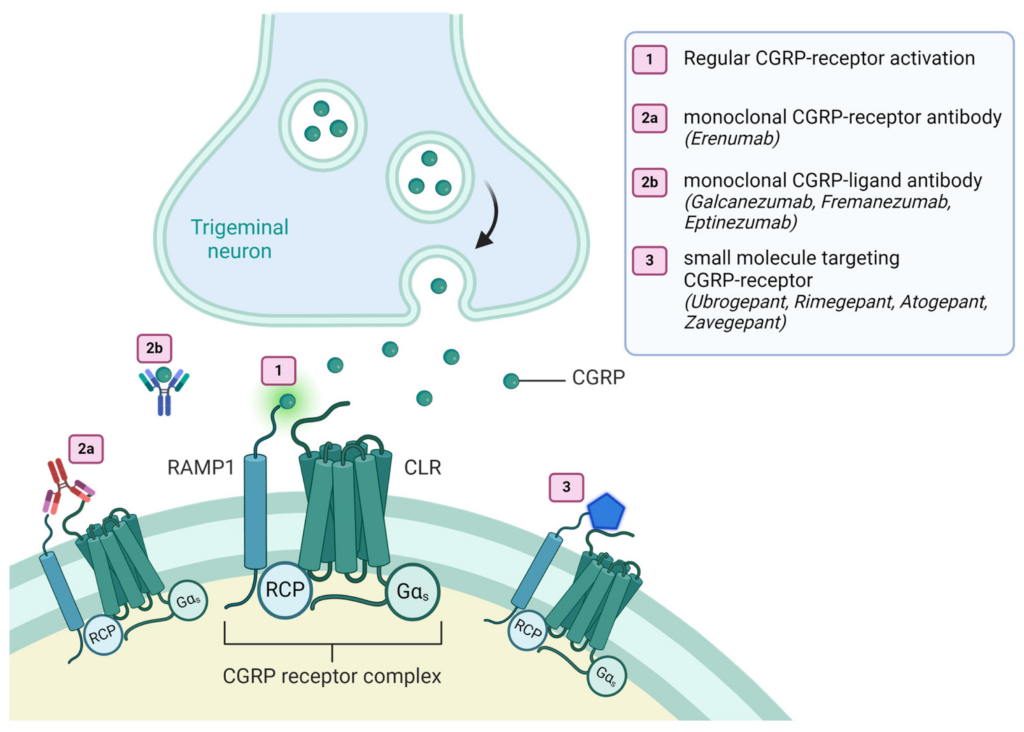
Figure 1. Targets of CGRP-targeting therapies at the canonical CGRP-receptor. (1) Illustrates the activation of the CGRP receptor complex by its endogenous ligand CGRP. (2a) Shows a mAb-dependent blockage of the CGRP receptor. (2b) Demonstrates a mAb-dependent binding of the CGRP ligand. (3) Shows an inactivation of the CGRP receptor complex due to small molecules (gepants). CGRP (Calcitonin-gene related peptide), CLR (Calcitonin receptor-like receptor), GαS (Gs alpha subunit), RAMP1 (Receptor activity modifying protein 1), RCP (Receptor Component Protein).
Source: Eller, M. T. et.al. (2024). Novel Calcitonin Gene-Related Peptide (CGRP) Interfering Migraine Therapies and Stroke—A Review.
The Vitamin D Connection
Interestingly, research has revealed an important connection between vitamin D and migraine:
- Prevalence: Studies show that many migraine sufferers have lower vitamin D levels than the general population. In fact, vitamin D deficiency is surprisingly common among chronic migraine patients.
- CGRP Regulation: Vitamin D appears to help regulate CGRP production and release. When vitamin D levels are low, there may be less control over CGRP, potentially leading to higher CGRP levels and increased migraine risk.
- Inflammatory Pathways: Vitamin D has anti-inflammatory properties that may help counteract the inflammation triggered by CGRP during migraine attacks.
- Treatment Potential: Some clinical studies have shown that vitamin D supplementation can reduce migraine frequency and severity in patients with vitamin D deficiency, possibly by influencing CGRP pathways.
- Seasonal Patterns: This connection may help explain why some people experience more migraines during winter months when sunlight exposure (our main source of vitamin D) is limited.
Other Migraine Correlations
Hormonal Connections
- Estrogen Fluctuations: About 75% of migraine sufferers are women, and many experience attacks around menstruation. Estrogen levels appear to influence CGRP release and receptor sensitivity, which helps explain why hormonal changes can trigger migraines.
- Puberty Impact: Many migraine cases begin during puberty, suggesting hormonal shifts play a role in initiating the condition, particularly in young women.
Genetic Factors
- Family History: Migraine tends to run in families. If one parent has migraine, their child has about a 50% chance of developing them. This suggests genetic factors influence CGRP regulation and migraine susceptibility.
- Specific Genes: Researchers have identified several genes associated with migraine, including some that affect ion channels in neurons and others involved in CGRP signaling pathways.
Neurotransmitter Connections
- Serotonin: Low levels of serotonin (another neurotransmitter) are associated with migraine attacks. Interestingly, serotonin and CGRP interact in complex ways, with serotonin sometimes inhibiting CGRP release.
- Glutamate: This excitatory neurotransmitter appears elevated in migraine patients and may trigger the cascade that leads to excessive CGRP release.
Environmental Triggers
- Barometric Pressure: Many migraine sufferers report weather sensitivity. Changes in barometric pressure may affect CGRP release in susceptible individuals.
- Sleep Disruption: Poor sleep quality correlates strongly with increased migraine frequency. Sleep disruption alters several neurotransmitter systems, including those regulating CGRP.
Gut-Brain Connection
Food Triggers: Certain foods containing substances like tyramine, phenylethylamine, and nitrates can trigger migraines in susceptible people, possibly by indirectly affecting CGRP release.
Metabolic Associations
Magnesium Levels: Low magnesium is associated with increased migraine frequency. Magnesium supplementation can help some patients, possibly by stabilizing neuron activity and influencing CGRP release.
Why This Matters
Understanding CGRP’s role in migraine, along with these diverse correlations, has transformed how we view this condition. Rather than seeing migraine as simply a blood vessel problem or a psychological issue, we now recognize it as a complex neurological disorder with specific biological mechanisms that can be influenced by multiple factors.
For migraine sufferers, this comprehensive understanding opens multiple avenues for treatment – from CGRP inhibitors to vitamin D supplementation to hormonal management to lifestyle adjustments. This integrated approach offers hope for better control of a condition that can significantly impact quality of life, education, and career opportunities.
The story of CGRP and migraine illustrates how scientific discoveries about specific molecules in the brain can lead to breakthrough treatments and a deeper understanding of complex conditions.
What can you do?
Based on our understanding of CGRP and these various correlations, here are practical steps you can take to help manage migraines:
- Monitor Vitamin D Levels: Consider having your vitamin D levels checked, especially if you live in areas with limited sunlight or experience seasonal patterns to your migraines. Supplementation may help if you’re deficient (always consult a healthcare provider first).
- Track Triggers: Keep a migraine diary to identify your personal triggers, particularly noting hormonal cycles, weather changes, sleep patterns, and food sensitivities. Many smartphone apps are available for this purpose.
- Maintain Regular Sleep: Establish consistent sleep and wake times to help regulate neurotransmitter systems that influence CGRP.
- Manage Stress: Practice stress-reduction techniques like meditation, deep breathing, or yoga, as stress can trigger CGRP release.
- Consider Magnesium: Magnesium-rich foods (dark leafy greens, nuts, seeds) or supplements may help some migraine sufferers.
- Stay Hydrated: Dehydration can trigger migraines in susceptible individuals.
- Moderate Exercise: Regular, moderate exercise may help reduce migraine frequency, possibly by affecting CGRP regulation and improving sleep quality.
- Mind Your Gut Health: Consider probiotics or dietary adjustments if you notice digestive issues correlating with your migraines.
- Limit Trigger Foods: Common triggers include aged cheeses, processed meats, alcohol (especially red wine), chocolate, and foods containing MSG or artificial sweeteners.
- Hormonal Awareness: For those with menstrual migraines, tracking cycles and discussing hormonal management strategies with healthcare providers can be beneficial.
Our books
Want to learn more about your Migraine and Migraine Management?
We make Migraine research more available for migraine sufferers. Through our books you will learn what might be causing your migraine and what you can do to reduce the number of migraine days and the intensity of migraine attacks. If you are not using a Migraine Tracker or Headache journal we recommend you start doing so – This is crucial if you are seeing a neurologist or a GP. The tracker helps you find out what kind of migraine (s) you have and what trigger them.
Note that all of our books are included in 90-days program without any extra charge. The books are available in national libraries in Norway.

Ebook
50 things you need to check
if you suffer from Migraine
if you suffer from Migraine
Ebook
Ebook / Print-on-demand
Track migraines effectively for neurologist insights and your own understanding.
Print-on-demand. Visit Lulu bookstore



