Migraine – the sum of many causes
For the body to function, we depend on the nervous system, hormones, blood circulation and digestion working together. These systems work together continuously, and it happens by itself. We don’t have to think about it. The systems are affected by genes, food, stress, sleep, physical activity and other mechanisms that we know are important for good health.
Migraines are affected by exactly the same mechanisms and systems. This is also the reason why in some phases of life we can be more sensitive to migraine triggers. If we sleep poorly, have forgotten to eat and are stressed, bright light is much more likely to trigger a migraine than if we are rested, relaxed and full.
It is very important to reflect on this. Although we may think that a given trigger always causes migraine attacks, this is not the case. If we have a good general health status, the body’s tolerance is higher and we are less sensitive to triggers. In fact, the fear of triggers alone can make us more sensitive to migraine attacks. A strategy to prevent migraines will be to accept the triggers, and do what you can to have surplus and good health. What you think is a trigger can also be part of the migraine attack. It can include hunger, thirst, fatigue and neck pain. Sometimes it is impossible to determine whether they are triggers or part of the migraine.
Allostatic Load
A word used to describe how to prevent and protect the balance in the body is allostasis. If you are in good health with a high tolerance for triggers and external stresses, you have good allostasis. If, on the other hand, you have weakened protection and burden your body with little sleep, stress and poor food, you have allostatic stress. Migraine is a very good example of a bodily challenge that is subject to allostatic stress.
One of the reasons why migraine patients are so sensitive to changes and imbalances in the body is due to the hypothalamus.
The hypothalamus is a small nucleus in the middle of the brain, and despite its small size, it helps to regulate important functions such as circadian rhythm, sleep, hunger, thirst and pain. The hypothalamus is central to migraine and cluster headaches in particular, as it regulates many of the connections between triggers and symptoms.
Knowledge of the function of the hypothalamus can perhaps contribute to increased motivation and understanding of what one can do to prevent migraines.
We will give some examples of what causes allostatic stress, and some of them are influenced by the hypothalamus.
Sleep
Many people with migraines have sleep problems that affect each other in both directions. Migraines can disrupt the quality of sleep, and sleep problems can cause migraines. In addition to negative consequences for the brain, poor sleep quality and too little sleep will affect the body in general, including increased appetite, increased risk of inflammation in the body, increased stress responses in the body, increased blood pressure and increased blood sugar and insulin. These bodily reactions will increase the allostatic load, which in turn will lead to a higher sensitivity and risk of migraine.
Migraines as well as cluster headaches are affected by the circadian rhythm. The hypothalamus helps regulate the circadian rhythm, for instants through the hormone melatonin. Good sleep hygiene (by going to bed and getting up at fixed times, a dark room when going to bed, and the right light in the morning) leads to better sleep, excess and a better balance between pain impulses and hormones via the hypothalamus, which in turn can prevent migraines.
Research from Harvard Medical School has shown that combining an approach like the Scandinavian Method with preventive medication works better than medication alone.
Food and hunger
The symptoms of hunger can resemble the prelude to a migraine attack. Sweating, pallor, yawning, lethargy and nausea are some of the similarities. It is the low blood sugar that triggers migraines when you are hungry. In fact, low blood sugar can also occur after eating too much sugar in a short time, due to overstimulation of insulin, which lowers blood sugar.
The hypothalamus is also central in this connection, and is important in the regulation of appetite.
The feeling of hunger can in some cases be a normal precursor to a migraine. Then food needs (“cravings”) may arise, including the desire for chocolate. When you eat chocolate, and you then get a migraine, it will be natural to blame the chocolate as a migraine trigger. Although the migraine attack was coming anyway. Of course, this does not apply to everyone. For some, chocolate is a real migraine trigger, but it’s worth noting that the research in this area is quite weak. In any case, it is a good idea to record eating habits and early symptoms in the headache diary to assess whether there is a fixed pattern or not.
To keep blood sugar stable, it is best to eat food with protein and fat at regular times, and limit sugary foods. Eating Ultra Processed Food could also contribute to not only Glycaemic variability, a higher risk of diabetes type-2, cognitive decline and earlier death it can also be the reason for your migraine. We have included a video under the section “Hormones”
Hydration and thirst
The hypothalamus also regulates the sensation of thirst. Again, the feeling of thirst can be a precursor to a migraine attack. But mild dehydration itself can also lead to migraines and other headache types, such as tension-type headaches. 8 glasses of water a day is a general recommendation. Remember that sugary drinks, tea and coffee can be diuretics, and thus do not maintain fluid balance in the same way as water.
Physical activity
Physical activity will contribute to better health in general and less stress, which in turn will prevent migraines.
Larger studies nevertheless show that those with migraine move too little, which means less than 150 minutes per week of moderate activity. For some, it may be due to a lack of knowledge about proper training or a lack of time and motivation. For others, it may be due to fear that movement will trigger a migraine attack.
A person with migraine may get more headaches during high-intensity exercise with a high heart rate. This is particularly true when you are already in a seizure, but some may also find that a high heart rate can trigger a headache. This is the opposite with someone with a tension headache, where physical activity should not worsen the headache. What many people forget is that exercise does not always lead to migraines. right guidance can make the big difference so that you get more security about your activity tolerance.
Physical activity:
- Improves health in general
- Reduces stress
- Improves sleep
- Often leads to good eating habits
- Increases pain tolerance
- Contributes to the production of endorphins and other hormones that prevent pain and illness
- Improves mood
All these factors will directly or indirectly contribute to fewer migraine attacks
Also remember that exercise, combined with manual treatment, has a good effect against migraines, especially when you also have tension headaches and neck pain. We can help you with this.
So how do you get started with the right training? The secret is to adapt the training with gradual progression.
Tension in the neck
Around 40% say pain in the neck can trigger a migraine attack. Neck pain can also be experienced together with headaches, without being a direct trigger. Around 80% have neck pain and headaches. There are more people with neck pain among those who have both migraine and tension headache (90%) than those with only migraine (75%).
The use of Botox can illustrate the connection between neck, shoulder and jaw tension and migraines. Botox (onabotulinumtoxinA) is used by many people with chronic migraines. Chronic migraine means that you have a headache 15 days a month, and 8 of those are migraines. Botox is typically placed in several places in the neck, shoulders, jaw and skull every 12 weeks to prevent migraines. It is assumed that Botox prevents signaling substances (including CGRP) that are central to migraine attacks. Botox also has a muscle-relaxing effect.
Relaxation, manual therapy, exercise, acupuncture and biofeedback reduce tension in the neck, shoulders and jaw, and are recommended to prevent migraines. Biofeedback is a self-help technique where you objectively measure tension in the muscles, and actively try to relax to see if the tension, and the pain, becomes less intensive. Many also have effect of acupuncture in the prevention of migraines. Manual treatment can help against migraines, especially in combination with exercise. Fitness training (aerobic training) proves to work well, especially when migraines are combined with tension headaches and neck pain.
Stress
Stress is listed as the most common trigger for migraines. When you have recurring pain and migraines, stress is part of the vicious cycle. Stress can trigger a migraine attack, and having a migraine can cause stress. In fact, changing from a normal everyday life with stress to a quieter life, for example during a holiday, can also lead to migraines. So how do you prevent stress? Everyone experiences stress at times in their lives. Often the source of stress is difficult to remove. Then it’s a good idea to consider how you can handle the experience of stress better. Again, you should prioritize building up a favorable allostasis. Good sleep hygiene and regular physical activity make you better equipped to cope with the sources of stress in life. With surplus and a clearer head, you may not want to think so much about the stress.
About 80% of people with migraines report stress as a trigger.
Mood
Having a good mood is positive for health, and can prevent migraines. Mood affects migraines, among other things, through serotonin. Serotonin is a signaling substance in the brain, but some people also know it as the happiness hormone. It is involved in depression and anxiety. In a migraine attack, serotonin is central and affects both nerves and blood vessels. Triptans are a well-known group of migraine medications that act as a kind of antidote to, among other things, serotonin.
Medicines
Medicines, both anti-seizure drugs and preventive ones, are absolutely necessary for many people with migraines. But you have to do it according to the right indications and not too often. If you use common painkillers such as paracetamol and ibux more than 15 days per month, or triptans more than 10 times per month for 3 months, there is an increased risk of getting headaches from the medicines. This is called medication overuse headache (MOH), and comprises 1-2% of the population. 80% of those who develop MOH have migraine. Too much and the wrong medication, just like too little sleep and stress, affects both the chemical and hormonal balance in the body. This can contribute to a change in pain tolerance and increase the chances of migraine attacks.
If you have migraines, medication must be planned in consultation with a doctor with knowledge of headaches. Use a headache calendar so you have control over attacks and medications. If the medicines do not have an effect, or you exceed the limits of recommended doses, you must contact your doctor to reduce the dose.
Hormones
Migraines have a clear hormonal component, particularly when estrogenlevels change. Estrogen has several important functions, among which it has a pain-relieving effect. Many women find that the migraine gets worse if menstruation, when the estrogen level drops, and improves with pregnancy, when estrogen levels increase. Some may experience improvement of the migraine with preventive hormone therapy.
Hormonal imbalance can occur in people as young as 30 years. However if may not only be a result of aging, but also lifestyle choices, such as a poor diet and lack of exercise. The standard American diet, which consists of approximately 60 % Ultra Processed Food, is a top contributor to early hormone imbalance (source: New York University).
Changes
As illustrated in several of the points above, migraine is sensitive to changes. This applies to changes in sleep, hormones, stress and many other unavoidable parts of life. Headache experts actually recommend that someone with migraine should strive to have as many fixed routines as possible and little physical or psychological variation.
Our Holistic approach
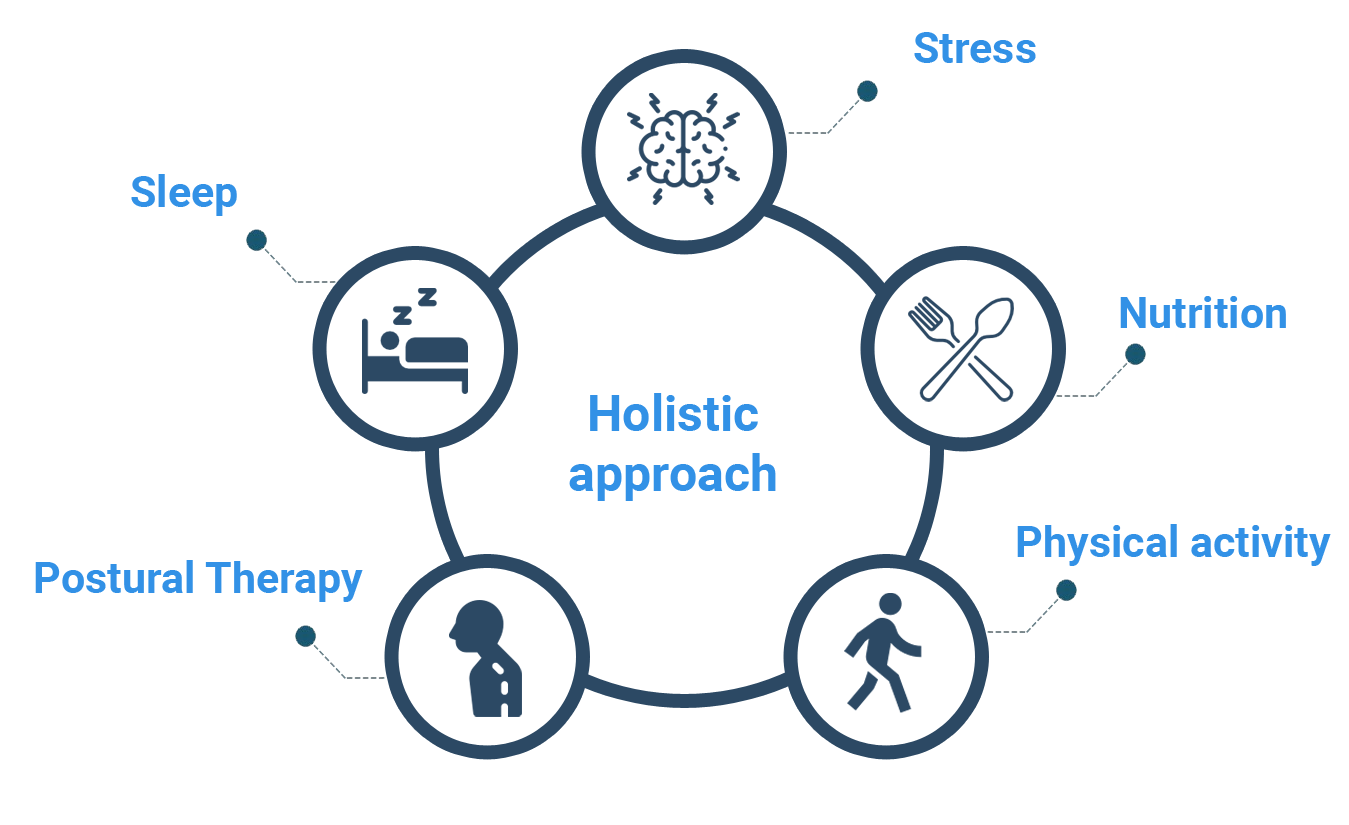
The Scandinavian Method uses a holistic approach. Through a thorough assessment we look for factors that is proven to cause migraine and tension-type headache. Here you can upload pictures of yourself and get help from our AI to analyze your posture.
After the assessment our system will create a personalized 90-days program. The program is science based and uses techniques that have been scientifically proven to reduce the intensity and frequency of migraine and headaches.
A holistic approach like this has also proven to help those who already are under medical treatments.
The program has been created by authorized health personell by the Norwegian government with over 15 years experience treating migraine and tension-type headache.
The Scandinavian Method is partly funded by the Norwegian government through Innovation Norway.
© Copyright. All Rights Reserved